07.13.23 • By Trevor Murphy & Ian Bernstein
*This article was previously posted on the Oscar tech blog
It’s no secret that healthcare in the US is confusing and hard to navigate, even for those of us that work in this industry!
There are many obstacles in an individual’s journey through the healthcare system, but among the largest is understanding how claims work. In service of Oscar’s mission to make healthcare more accessible, we decided to take a deeper look into how our customer service teams support our members as they attempt to better understand the claims lifecycle. All Oscar members are supported by our Care Team, allowing them to call in and get help with any issues or questions they may have about their insurance.
After analyzing phone calls between members and their Care Teams, we noticed that claims-related topics consisted of 16% of calls to Oscar, and these calls were among the longest and most complex for our teams to manage. The Care Team is staffed with Care Guides who leverage a homegrown inbound support tool called Rosco to help answer member questions. In order to better support our Care Guides in answering member questions related to claims, we embarked on a multi-pronged Rosco enhancement initiative which has led to positive feedback from our Care Guides.
Throughout this post we’ll explore how we landed on the claims lifecycle as a problem to solve and take you through our process of aligning on the right solution to help our Care Guides successfully explain/navigate the confusing claims landscape for our members. Building software is nothing if not collaborative so in that spirit Ian Bernstein, the Product Manager for this project, and Trevor Murphy the Designer, will partner to walk you through every step of our journey.
It’s no secret that healthcare in the US is confusing and hard to navigate, even for those of us that work in this industry!
There are many obstacles in an individual’s journey through the healthcare system, but among the largest is understanding how claims work. In service of Oscar’s mission to make healthcare more accessible, we decided to take a deeper look into how our customer service teams support our members as they attempt to better understand the claims lifecycle. All Oscar members are supported by our Care Team, allowing them to call in and get help with any issues or questions they may have about their insurance.
After analyzing phone calls between members and their Care Teams, we noticed that claims-related topics consisted of 16% of calls to Oscar, and these calls were among the longest and most complex for our teams to manage. The Care Team is staffed with Care Guides who leverage a homegrown inbound support tool called Rosco to help answer member questions. In order to better support our Care Guides in answering member questions related to claims, we embarked on a multi-pronged Rosco enhancement initiative which has led to positive feedback from our Care Guides.
Throughout this post we’ll explore how we landed on the claims lifecycle as a problem to solve and take you through our process of aligning on the right solution to help our Care Guides successfully explain/navigate the confusing claims landscape for our members. Building software is nothing if not collaborative so in that spirit Ian Bernstein, the Product Manager for this project, and Trevor Murphy the Designer, will partner to walk you through every step of our journey.

Problem
There are countless quality of life improvement related problems to tackle at Oscar, so why invest the time and resources into streamlining the claims experience for our Care Guides? To answer that, it’s first important to understand that Oscar is a technology first company where we own the entire stack of technology we use, and part of that is building our own custom solution for claims processing. This new solution is the result of a long development process, but it now enables us to effectively scale our business, takes advantage of many administrative efficiencies, and establishes a strong foundation upon which we can continue to differentiate and build innovative capabilities. Our brand new claims system was ready for rollout which meant that the timing was serendipitous for us to unlock everything the new platform had to offer, including enabling our Care Teams more visibility into claims in Rosco.There were two primary reasons to dig further into how Rosco would support the the new platform change
- We realized that the infrastructure was aging and needed a refresh, and
- Claim calls can be complex, and they have always been longer in duration and more difficult to handle than other types of member or provider inquiries.
Claims are submitted after a procedure is conducted. They get processed through our system based on eligibility and codes submitted to a payer from a provider. The claim can then be updated over time as well through adjustments as a provider shares new information like updated codes, medical records, or submits for retroactive prior authorizations. These nuances make it more challenging for our Care Teams to accurately represent to members how a claim moves through the lifecycle.

User needs
We knew the front end of our application was going to need to be updated to support this new claims processing system. This offered the perfect opportunity for us to invest in understanding our Care Team’s needs more deeply and learn where the current experience was painful or needed improvement. We began this fact finding mission moving up the initial edges of the double diamond design process in an effort to cast a wide net and learn all we could. We started by conducting group sessions with Care Guides to gather an initial understanding of the space. We then set up time to shadow live calls that Care Guides were fielding from members to see how Rosco was being used, set up one on one interviews for deep dives, and sent out surveys to all teams that would be impacted by our work. We also worked directly with internal teams to get a better understanding of what information was available today and what new data we could begin to leverage once our migration was complete. Through all of that we learned a lot and were able to align as a team on the four largest problem areas to solve for:1. Historical adjustments made to claims are hard to understand:
There are times where a claim may need to be processed again and some back and forth is needed between a provider and a payer. This results in a claim changing over time and the original tool we were using didn’t effectively assist our Care Team in visualizing and explaining these changes to our members.
2. Lack of a holistic picture creates a disjointed experience:
Oscar’s initial claim system was hyper focused on medical claims and that same focus was apparent in the tooling our team was using. Our users were asked to leverage external tools from our Pharmacy Benefits Manager in order to answer member questions related to pharmacy, which added time and complexity to calls.
3. Member expectations don’t align with how claims were processed:
An individual navigating healthcare expects the date they received care to be the date that claim was processed, but the fact is that claims can be delayed for any number or reasons resulting in a misunderstanding of how something like a deductible was impacted.
4. Raw data available in Rosco requires manual synthesis to answer members questions:
Our tooling was focused on delivering the data from a single claim, but where it came up short was in helping to translate that data into knowledge that our team could use to answer member questions. We wanted to make it easier to answer simple questions like, “when did I meet my deductible?” without forcing our team to jump through hoops.
Pulling pieces together
To tackle a problem as massive as this one, we needed to work cross functionally, involve our users, and wrangle complex data.
Our Care Team users that were impacted by the changes within our claims experience were instrumental throughout this project. We had frequent conversations with our users on changes we were experimenting with to ensure the changes aligned with their needs before they were implemented. We were in lock step with our stakeholders so they knew what to expect before the changes were implemented and could therefore successfully prepare for the change.
- Cross team collaboration: We worked closely with the teams that own claims data, our customer service team users, and the technology teams. The information we display in our Care Team application is only as good as the data we get from the teams that provide it to us.
- Involving our users: We worked extensively with our internal teams to ensure that as they were building the new claims processing system, they were building with the business and the user needs in mind. It’s very easy to get lost in building a complex system and finding out afterwards that the system isn’t helping the front line teams that need it the most, so we sought to remove those obstacles through constant communication and incremental builds.
- Wrangling complex data: There is a lot of data associated with getting a claim processed correctly. We needed to work closely with our technology teams to make sure that we could successfully pull in data from various sources and ensure the front end experience wouldn’t break. We constantly asked ourselves how we could build the front end experience in a way that uses microservices to solve our pain points, reducing the load on the system that would be necessary to display the critical information for our users.
Our Care Team users that were impacted by the changes within our claims experience were instrumental throughout this project. We had frequent conversations with our users on changes we were experimenting with to ensure the changes aligned with their needs before they were implemented. We were in lock step with our stakeholders so they knew what to expect before the changes were implemented and could therefore successfully prepare for the change.
Updating the UI
After a thorough series of iterations and testing we finally arrived on an update to our existing solution that honed in on solving our users’ pain points. The tool we were designing for wasn’t one we personally use every day, so putting ideas and new designs in front of actual end users to gather insights and feedback was a crucial part of our journey in making claims easier to understand.
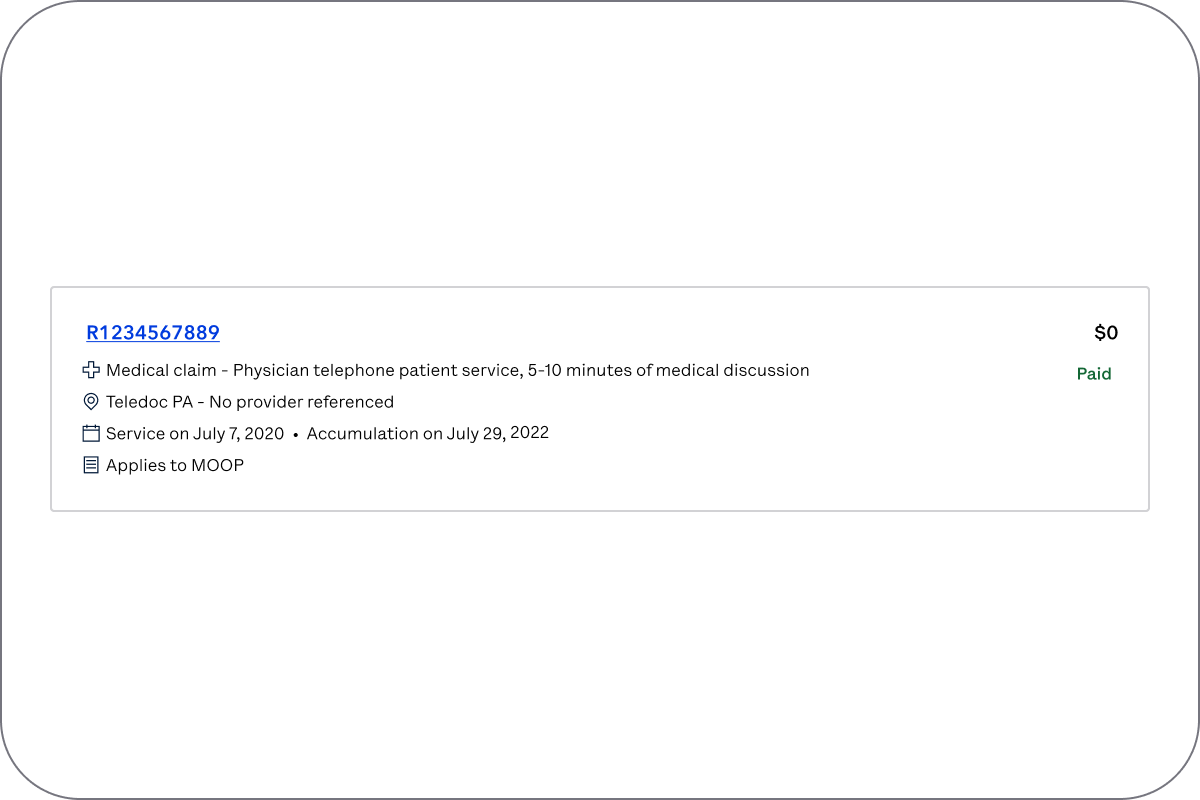
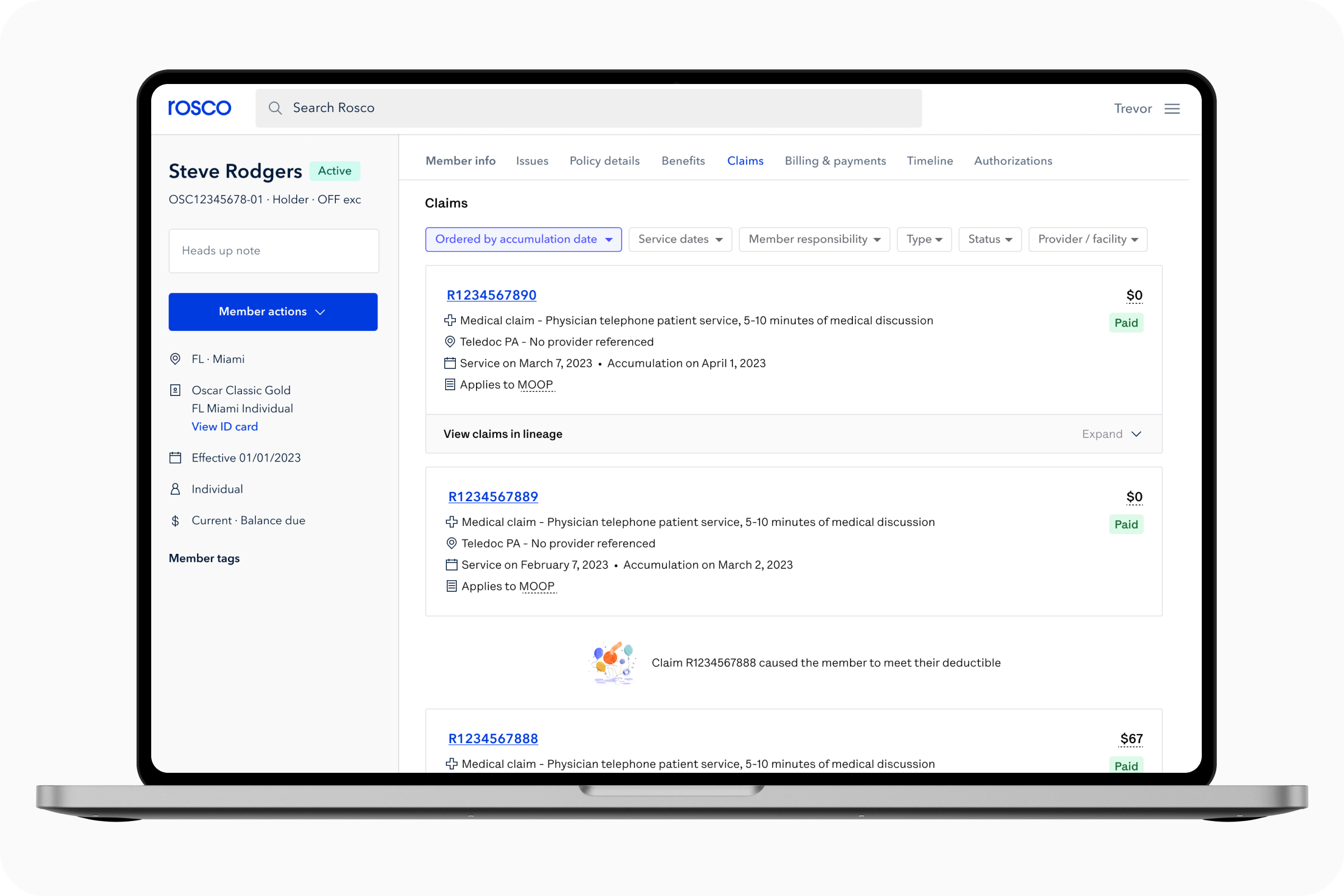
Change number 1: Cards > Tables
We opted to move away from a table based solution and instead custom built cards designed specifically for claims. These cards now surface all relevant information that was initially hidden behind a click and allow the Care Guide to locate a claim quickly. Additionally, data is now placed in a consistent vertical view area which makes it easy to scan while scrolling down the page.
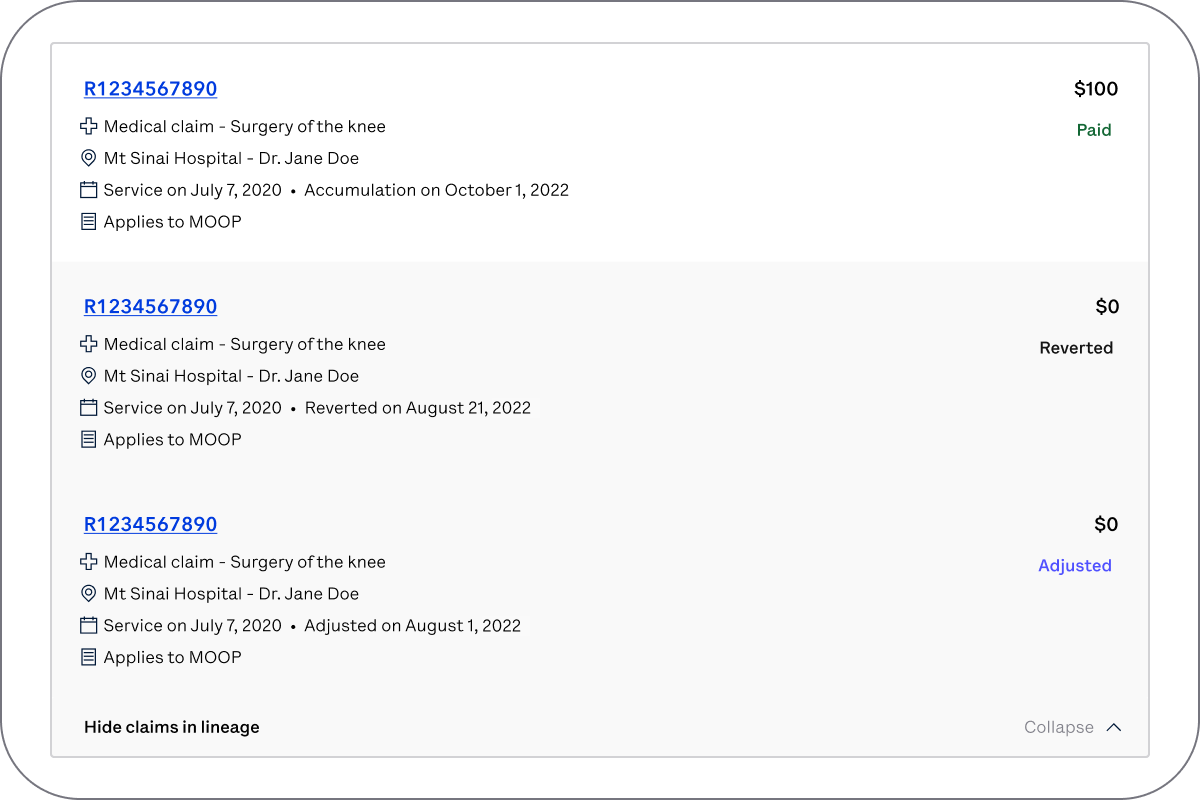 Change number 2: Collapsing adjustments
Change number 2: Collapsing adjustmentsOur claims card now has the ability to collapse historical information behind it so rather than having a new claim for each possible adjustment, now the most up to date information will always be shown up front while the historical context is a click away.
 Change number 3: Answering common questions
Change number 3: Answering common questionsTo create a clearer connection between the claims themselves and a member’s accumulators (deductible) we now show what we’re calling a ‘pillow’ UI to help take some of the guesswork out of the equation. The pillow tells someone the outstanding balance of a deductible and once met is a secondary affordance that will eventually point the user to the claim that caused it to be met. Further down the page our claims can now be sorted not only by date of service, but also by the date the claims processed. This makes it easy for us to now surface in-line notifications amongst our claims which focus on calling attention to key events, like when a deductible was met.
 Change number 4: Support for non medical claims
Change number 4: Support for non medical claimsWith new service support available, showing a holistic picture of a member’s care was now possible so we adjusted our claims card to support it. Relevant pharmacy data becomes available in claims cards and new iconography helps a user understand claim type. Vision, dental, and mental health services are all covered in this same way!
What does impact look like
To ensure that what we built was providing value to our users, we leveraged two primary metrics to assess impact:- Successful completion of our back-end migration such that we only rely on the new infrastructure/system for our claims experience. This creates a more reliable system/experience for our users and enables us to implement new UI changes to solve major pain points.
- Improvements in overall efficiency for our users that interact with the new claims experience. We worked closely with our Data Science team to discuss metrics we could track to analyze the success of this project. We were hoping to achieve a reduction in the number of inquiries that get escalated to another team to solve as well as a decrease in the amount of time it takes a user to answer claim related questions.
Given how closely tied these success metrics were to Oscar’s overall goals of reducing confusion for members and costs of running our business, we were able to successfully prioritize this work in our annual product roadmap. Since March of 2022, we’ve been releasing changes in phases and testing how each phase impacts our core metrics as a part of our build, measure, learn product cycle.

Pilot and change management
Although we had reasonable confidence that we built the right thing, we wanted to make sure we had controls in place to ensure our new features worked well for our Care Guides. We created one last round of feedback in the form of a beta launch. We worked with our stakeholders to identify a diverse set of beta users so we could have assurance that the solution was working for all users, since many of our users have different needs.This pilot group was used for a tight change management approach. These users had access to the new solution for two months to ensure the functionality was working as expected and give them an opportunity to provide feedback. We created a test and control group across this group and all other users to help us measure the effectiveness of the new design.
Then we reviewed the feedback, and were able to make changes to the functionality before launching to all users. Simultaneously we monitored our core metrics to ensure that pilot users were experiencing a reduction in call time which has positive impacts on service performance.
Out in the wild
We are continuing to gather feedback so we can make the experience even better and are monitoring the data so we can ensure the claims experience is continuing to yield positive benefits.Looking ahead, we’re also planning to incorporate AI as we highlighted in our continuous hackathon site.
This project is only one of many that we are focused on that addresses internal tool enhancements to drive business value by improving the experience of our stellar Care Teams that are on the front lines with our members every day. Although we are only a piece of the puzzle, we are excited to be doing our part and help Oscar achieve profitability and reduce the complexity of the US healthcare system for our members!
Trevor Murphy is a Senior Product Designer, currently leading design for all teams in the Provider & Clinical space. Previously supported design needs for our customer service tools.
Ian Bernstein is a Product Manager at Oscar, working on our Customer Service tools.
